Reviewed by Lexie CornerDec 9 2024
According to a study published in Oncogene, an MRI-based imaging technology developed at the University of Cambridge predicts the response of ovarian cancer tumors to treatment and provides a rapid assessment of treatment effectiveness in patient-derived cell models.
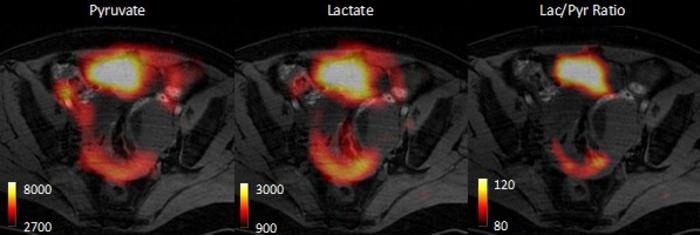 These images, from a small-scale unpublished study in human ovarian cancer patients, were created using a technique called hyperpolarized carbon-13 imaging that allows doctors to distinguish between different subtypes of ovarian cancer, to reveal their sensitivities to treatment. The scientists observed different rates of pyruvate conversion into lactate in different tumor deposits, suggestive of the presence of different tumor subtypes. Image Credit: Kevin Brindle/ University of Cambridge
These images, from a small-scale unpublished study in human ovarian cancer patients, were created using a technique called hyperpolarized carbon-13 imaging that allows doctors to distinguish between different subtypes of ovarian cancer, to reveal their sensitivities to treatment. The scientists observed different rates of pyruvate conversion into lactate in different tumor deposits, suggestive of the presence of different tumor subtypes. Image Credit: Kevin Brindle/ University of Cambridge
This technique, hyperpolarized carbon-13 imaging, can enhance the signal detected in an MRI scanner by up to 10,000 times. Researchers found that this method can differentiate between two forms of ovarian cancer, indicating their varying susceptibility to treatment.
The team applied it to patient-derived cell models that closely mimic human high-grade serous ovarian cancer, the most common and deadly type. The imaging method effectively identifies whether a tumor is sensitive or resistant to carboplatin, a standard first-line chemotherapy drug for ovarian cancer.
This technology allows oncologists to assess how well a patient is responding to treatment and track its effectiveness within the first 48 hours.
Ovarian cancer subtypes respond differently to treatments, and current testing often requires weeks or months to determine if a treatment is working. This imaging method offers faster results, enabling oncologists to adjust and personalize treatment plans within days.
In comparison to Positron Emission Tomography (PET), a widely used clinical tool, the study showed that PET could not detect metabolic differences between tumor subtypes, and therefore could not predict the type of cancer present.
This technique tells us how aggressive an ovarian cancer tumor is, and could allow doctors to assess multiple tumors in a patient to give a more holistic assessment of disease prognosis so the most appropriate treatment can be selected.
Kevin Brindle, Study Senior Author and Professor, Department of Biochemistry, University of Cambridge
Ovarian cancer patients often have multiple tumors spread across their abdomen. Performing biopsies on all of these tumors is not feasible, and they may vary in subtype, each responding differently to treatment. MRI is a non-invasive method, and the hyperpolarized imaging technology allows doctors to assess all lesions simultaneously.
Brindle added, “We can image a tumor pre-treatment to predict how likely it is to respond, and then we can image again immediately after treatment to confirm whether it has indeed responded. This will help doctors to select the most appropriate treatment for each patient and adjust this as necessary. One of the questions cancer patients ask most often is whether their treatment is working. If doctors can speed their patients onto the best treatment, then it’s clearly of benefit.”
The researchers expect to test the approach on ovarian cancer patients over the next few years.
Hyperpolarized carbon-13 imaging uses an injectable solution containing a ‘labeled’ version of the naturally occurring molecule pyruvate. Once in the body, the pyruvate enters cells, and the scan measures the rate at which it is metabolized into lactate. The metabolism rate reveals the tumor’s subtype and its potential susceptibility to treatment.
This study adds to the growing body of evidence supporting the broader clinical application of hyperpolarized carbon-13 imaging.
Brindle, also affiliated with the Cancer Research UK Cambridge Institute, has spent the last two decades refining this imaging technique to study various malignancies, including breast cancer, prostate cancer, and glioblastoma, an aggressive brain tumor with multiple subtypes and varying metabolic patterns that can be monitored to predict treatment response. The first clinical research at Cambridge, published in 2020, focused on breast cancer patients.
Every year, around 7,500 women in the United Kingdom are diagnosed with ovarian cancer, with approximately 5,000 cases being high-grade serous ovarian cancer (HGSOC), the most severe form.
The overall cure rate for ovarian cancer is low, with only 43 % of women in England surviving five years after diagnosis. Symptoms are often overlooked, allowing the disease to spread before detection, which complicates imaging and treatment efforts.
The study was funded by Cancer Research UK.
Journal Reference:
Chia, M. L., et. al. (2024) Metabolic imaging distinguishes ovarian cancer subtypes and detects their early and variable responses to treatment. Oncogene. doi.org/10.1038/s41388-024-03231-w